Rotator Cuff
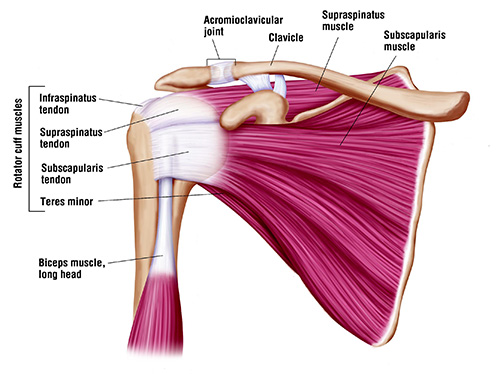
Anatomy: The rotator cuff is a group of four delicate tendons that holds the ball in the socket in the shoulder joint to allow the larger muscles (deltoid, pectoral major, latissimus dorsi) to move the joint.
Injury: The Supraspinatus, the tendon on top, tears first. The tear can then spread backward into the infraspinatus and then forward into the subscapularis. The fourth tendon, teres minor, does not normally tear. The tendons first tear partially underneath, before tearing completely and retracting. Repetitive overhead use of the arm over a period of years causes thinning of the tendons. Ultimately a minor elevation or strain completes the tear.
Diagnosis: Pain is felt to the side of the shoulder and down the side of the arm in most cases. Pain may also be in front, which may indicate biceps injury. Arm elevation causes pain and weakness. Pain is typically worse at night with complete tears.
Treatment
Partial tears: While many surgeons treat surgically, I have excellent success treating tendinitis and partial tears with PRP injection along with Physical Therapy, thus avoiding surgery for my patients many of whom have had recommendations for surgery elsewhere.
Complete tears: A completely torn Rotator Cuff tendon cannot heal and requires surgery, the earlier the better. With delays the tears increase in size and may become too large to repair necessitating shoulder replacement. I have decades of experience using minimally invasive arthroscopic repair for even the most complex cases. In fact I frequently repair tendons that have failed repair elsewhere. Tiny bioabsorbale suture anchors are embedded into the humeral head, the “ball” and then the tendons are cinched back in place using sutures attached to it. No immobilization is necessary afterward, although lifting is restricted while healing occurs.
Superior Capsular Reconstruction (SCR) For Irrepairable Rotator Cuff Tear Until now when rotator cuff tears were torn too severely for repair the only alternatives were so called reverse shoulder replacement, a massive operation without proven long term results. However a new procedure, SCR, - developed by top Shoulder Surgeon Dr. Stephen Burkhart in San Antonio - restores a newly discovered ligament at the top of the shoulder and can restore function and relieve pain in these patients. I recently spent time in San Antonio with Dr Burkhart to learn nuances of the procedure from him and now offer it to my patients in Chicago.
I DO NOT USE NERVE BLOCKS FOR SHOULDER SURGERY – HERE’S WHY
Unlike many shoulder specialists I prefer not to use nerve blocks for surgery – for several reasons.
- First, these are minimally invasive procedures for which nerve blocks are simply not necessary in my hands. We have found that the use of motorized ice machines combined with a short period of narcotic use are satisfactory. Indeed some patients hardly even need the narcotics because of the benefits of the cold therapy.
- Second, numerous studies and meta-analyses, including a new just published such study have shown that there is a “rebound effect” that results in greater pain the day after surgery than if no block were used. Years ago I tried using blocks and noticed that my day-after surgery patients were often miserable, worse on average than patients who had no block, and I stopped using them – as has been reported in numerous published studies.
- Third, the blocks do provide better pain relief for 6-8 hours after surgery facilitating patients being discharged. However when the block wears off late at night the pain can be difficult to control. I took care of patient a few years ago who had failed prior surgery in at a respected major medical center. His pain was so severe when the block wore off the night of surgery that he passed out and had to be taken by ambulance to the hospital. He was quite unhappy. If he had not had a block this excess pain would been recognized before he left and could have been properly controlled, perhaps he would have been admitted. As it stands the block benefits the hospital or surgicenter by allowing them to discharge patients on time but is not always in the patient’s best interest.
- Fourth, although rare, complications from blocks, such as nerve damage do occur – and I have seen such patients referred in. In my view there is no reason to take even small risks for a procedure that offers no significant compensatory benefit, and, as described above, is in fact undesirable in my opinion for the other reasons described above.
I wish to add that the use of nerve blocks for those surgeons who choose to use them is perfectly appropriate and I respect their judgement, but the above evidence based discussion explains why I believe it is in my patient’s best interest not to use them in general. I would add that in special circumstances, such as medication allergies, I will use them. And I will also use them if the patient wishes me to, although in my experience most patients are relieved at not having to have one. My goal is to have an informed evidenced based discussion with the patient so that we can make the best decision for that individual together.









