The Patient's Comprehensive Guide to the ACL
See Also ACL Reconstruction
About This Book
It is the purpose of this book to provide a comprehensive reference for the patient with a torn ACL. The information in it is based on the scientific literature but presented in a form that the non-physician can understand. I have attempted to provide information about which there is general consensus within the medical community. At the same time I have included specific information about my own techniques and preferences and identify them as such. I believe that patients are capable of understanding more than we physicians sometimes realize and therefore have tried to err on the side of “too much information” to allow you, the reader, to pick and choose. As the editor of the first comprehensive medical textbook on the ACL I have been fortunate to sift through virtually the entirety of ACL related scientific knowledge. This has resulted in an 84-chapter textbook with fifty contributing ACL experts from around the globe beside myself which is now in publication and will be released to the worldwide orthopaedic community in September of 2007. I have not included information here that is strictly related to surgical technical matters, and have combined some other topics to produce the 20 chapter work product below. My hope is that it will allow persons in need of ACL related knowledge to spend their time reading the scientifically valid information presented here and less time searching the internet trying to find it.
1. The Structure and Function of the ACL
3. Incidence by Gender, Sport, and the Presences of an ACL Injury Prevention Program
4. Why Do Females Tear Their ACLs More Than Males?
6. Diagnosis
7. Non-Operative Treatment of ACL Tears
8. Arthritis Formation After Unreconstructed ACL Tears
9. The Economics of ACL Reconstruction
10. Graft Choice and Graft Strength for ACLR
13. Ligamentization and Graft Tunnel Healing
14. Revision ACLR: Reconstruction After Failed Initial Surgery
15. ACLR In the Children Who Are Still Growing
16. The Treatment of Partial ACL Tears
17. Treatment of Associated Injuries
18. Post Operative Course and Rehabilitation
19. Restoration of Hamstring Strength
20. Stability Results After ACL Reconstruction
21. Complications and Problems
Introduction
Tear of The Anterior Cruciate Ligament (ACL) is the most important Sports Medicine injury. This is because failure to reconstruct a torn ACL usually leads to both an inability to satisfactorily participate in vigorous activities and the gradual deterioration of the knee, often resulting in total knee replacement at a young age. ACL tear is also important because its satisfactory treatment is almost always surgical; and because partial or complete failure of surgical treatment is relatively common. Indeed, restoring the cartilage that is damaged when the ACL is torn or when ACL reconstruction fails is even more complicated than the ACL reconstruction itself; and has helped spawn a new orthopaedic subspecialty of cartilage repair. The high profile nature of athletes who experience ACL tear further emblazon it in our consciousness. Finally ACL tear is important because it is quite common: with an estimated 125,000 ACL reconstructions to be performed in the United States this year at a combined cost to the economy in the billions of dollars.
The Structure and Function of the ACL
STRUCTURE
The ACL is about as big around as the little finger and runs more or less down the center of the knee. It is one of four ligaments (ligaments stabilize joints) connecting the tibia or leg bone and femur or thigh bone. In aggregate it maintains a relatively constant length as the knee bends and straightens. However different areas within it, the anteromedial and posterolateral bands, become more or less taut during these motions. This has generated a new approach to ACL reconstruction, double bundle repair, which will be discussed later. This anatomical fact has further significance regarding partial ACL tears, also discussed later on. The ACL is about three centimeters (two and a quarter inches) long. Its tibial attachment is closer to the front of the knee and its femoral attachment is closer to the back or posterior of the knee. It is this posterior attachment which results in ACL tear often producing pain in the back of the knee since the ACL almost always tears from its femoral attachment. The other three ligaments in the knee are the posterior cruciate ligament (PCL), which crosses the ACL – hence the word “cruciate.” – which is a little thicker than the ACL and rarely tears; the medial collateral ligament (MCL) which runs down the inside of the knee and is not infrequently torn at the same time that the ACL tear occurs; and the lateral collateral ligament (LCL) which tears only very rarely. Treatment of these other structures will be discussed in chapter 16.
FUNCTION
The ACL holds the knee together during pivoting and cutting and when landing after jumping. The posterolateral band tightens when the knee straightens, whereas the anteromedial band does not.
Contraction of the quadriceps muscle in the thigh when the knee is flexed (bent) to about 50 degrees or less, pulls the tibia forward powerfully with respect to the femur. The ACL, which runs primarily in a forward and backward direction resists this motion. When the knee is stressed during pivoting or landing there are forces tending to subluxate (partially dislocate) the knee. The ACL resists these forces, keeping the tibia in line with the femur.
Nerve endings within the ACL also help the body to subconsciously know the position of the leg during movement. This position sense is called “proprioception.” When the ACL is torn this position sense function from the ACL is also lost. It is not clear how significant this proprioceptive loss is and how much ACL reconstruction restores it (see Chapter 17 on Rehabilitation).
Mechanisms of ACL Injury
There is some controversy within this topic which will be discussed below. ACL tears clearly occur via one of two mechanisms: “contact” or “non-contact”. Contact injuries are less common but more clearly understood. This is the classic “clipping” injury from football in which the knee is hit from the outside during running. This is called a “valgus” blow and causes the knee to buckle inward. Both the ACL and MCL may tear as well as one of the cartilaginous menisci within the knee. It has become clear in recent years, however, that non-contact injuries are more common. This is at first counter-intuitive since ACL tear is known to be a severe injury and the more dramatic contact mechanism seems more appropriate to cause a severe injury. However non-contact injuries do indeed cause the vast majority of ACL tears.
With the large number of ACL tears that have been directly witnessed and with a great number of them have been filmed during athletic competition, it is surprising – but true – that we are still not sure exactly how the ACL tears. We know in a general way what happens but there have come to be two camps differing as to which force is the dominant one in producing the tear. The first is the “valgus” force described above. It is clear that valgus force strains the ACL. However the valgus force strains the MCL even more and it is difficult to understand how a valgus force by itself can completely tear the ACL without concomitantly tearing the MCL: however this is exactly what happens in most cases of ACL tear. I.E. the ACL is torn while the MCL is not injured.
The other force that strains the ACL is a strong, relatively unopposed quadriceps muscle contraction. This is a little harder to understand. The quadriceps muscle is the four part muscle that makes up the front of the thigh. It is the largest muscle group in the body. The function of the quadriceps is to straighten the knee. When it contracts it thus exerts a powerful force on the tibia when the knee is bent or “flexed.” This force can be divided into different components, if you remember your high school physics. One of the components tends to pull the tibia forward with respect to the femur: this is called “anterior translation”. The quadriceps muscle is so powerful that a near maximal contraction can generate enough force through this mechanism to actually rupture the ACL. There is no question that this mechanism contributes to ACL tear. The controversy is whether this force is secondary with valgus being primary, or whether this anterior translational force is primary with valgus being secondary, or whether the quadriceps can cause ACL tear entirely by itself with no valgus component. Obviously the mechanism of ACL tear varies from injury to injury and it is possible that all three mechanisms are operational in different circumstances.
The quadriceps force component tending to induce ACL tear, anterior translation, is stronger the straighter the knee becomes and disappears entirely when the knee is flexed to about fifty degrees. The time when the quadriceps contracts most powerfully is generally during landing after jumping. Putting this together it would be expected that landing after jumping when the knees do not flex very much at the time of landing would be the highest risk mechanism for quadriceps induced ACL tear. And it turns out there is now significant biomechanical evidence linking relatively stiff legged landing with an increased risk of ACL tear. In fact, as will be discussed in greater detail in Chapter 3, there is now some evidence that the greatly increased incidence of ACL tears that is found in females as compared to males may occur because females tend to land with less knee flexion – i.e. more stiff legged – than males.
The search for the actual mechanism of non-contact ACL tear is of more than academic interest. A clear understanding of this mechanism is an important component in the design of strategies to prevent ACL tears from occurring.
Incidence of ACL Tear by Gender, Sport, and the Presence of an ACL Injury Prevention Program
The overall incidence of ACL tear is unknown. Our best estimate comes from extrapolating from the incidence in Sweden. A registry is kept of all ACL tears. This was most recently found to be 6,000 tears per year for a country of 9,000,000 people, or one per 1,500 people. Extrapolating this to the United States would indicate that there are roughly 200,000 annual tears.
It has been known for more than a decade that females have a higher incidence of ACL tear than males. Why this is so is fully discussed in Chapter 4. It is also clear that some sports have a much higher incidence of ACL tear than others. Finally there have been a number of programs devised to decrease the incidence of ACL tears: these are fully discussed in chapter 5. However the actual variation in incidence as a function of gender and sport has not been well understood and the quoted rates vary widely. For example the increased incidence of ACL tears in females versus males was said to be nine to one in a recent Chicago Tribune newspaper article in a quote attributed to a physician. Is the number really this high?
We acquired and analyzed every article published in the peer reviewed scientific literature that we were able to identify regarding the incidence of ACL tear and performed a statistical analysis of the results: a so called “meta-analysis“. From this we were able to determine what the real numbers are regarding the female/male ACL tear incidence, the risk of ACL tear by sport, and where ACL tear prevention programs have proven to be helpful.
Why Do Females Tear Their ACLs More Than Males?
When it became clear that females indeed do tear their ACLs more frequently than males many hypotheses were put forth as to why. Over the last ten years or so these have subjected to critical analysis. Unfortunately the earliest hypotheses have been largely disproven but have become somewhat widely accepted as causative nonetheless. The potential causes for the gender disparity can be largely divided into three categories; structural or anatomic differences between females and males, physiologic differences, most notably hormonal differences, between females and males; and finally biomechanical or functional differences between females and males in the way they move and use their knees. We will refer to these as structural, hormonal or biomechanical respectively.
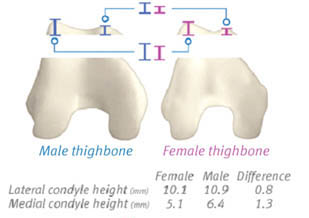 Intuitively it seemed most likely that structural differences – i.e. that females have thinner ligaments or a thinner “notch” where the ligament sits in the knee that tends to “guillotine” the ligament during injury would be the cause. And to this day it is widely held in both the medical and non-medical community that this is the cause. And while it may seem obvious it also appears to be false.
Intuitively it seemed most likely that structural differences – i.e. that females have thinner ligaments or a thinner “notch” where the ligament sits in the knee that tends to “guillotine” the ligament during injury would be the cause. And to this day it is widely held in both the medical and non-medical community that this is the cause. And while it may seem obvious it also appears to be false.
Females do have smaller ligaments and narrower “notches” than males. However they also, on average, have smaller knees. If the decreased ligament and notch sizes are normalized to their overall slighter stature there appears to be no difference between females and males. Thus, structural or anatomic factors do not seem to be the cause.
Prevention Programs
There have been numerous attempts over the years to devise programs that would hopefully reduce the incidence of ACL tears. It is difficult to judge the efficacy of these programs because the overall incidence of ACL tears is low. Thus the study must be quite large to detect a significant decrease in the incidence of tears. The most notable success in this regard is the study by Dr. Bert Mandelbaum and his associates. They showed that the incidence of ACL tear could be reduced by the institution of a program they called the “PEP” program that emphasized strength, flexibility and technique.
Diagnosis
Medical diagnosis is always the product of evidence from the history, physical exam, and diagnostic tests. We will go through each of these in turn. It should be pointed out that the diagnosis of ACL tear is difficult and tears are often missed in emergency rooms, by primary care practitioners and even by orthopaedic surgeons.
History: The most common history is a twisting injury, landing after jumping or being hit from the side (the football “clipping” injury). There is usually but not always marked swelling within six hours. The patient will often but not always hear or feel a “pop.” In about half of the patients cartilage is torn at the time or ACL tear and in half it is not. If cartilage is torn the patient will usually have persistent pain and follow up with an orthopaedist who will diagnose the torn ACL. However, if no cartilage is torn the patient will be very sore for from several days to one or two weeks but will then begin to feel better. If their tear has not been picked up by a physician during this time the patient may conclude that they had only a “sprain” and do not need medical treatment. They will then begin to function more normally for the next six months or so but will usually avoid athletics during this time because they sense some instability. However after six to nine months the patient may feel fine and begin pivoting activities again. When they do the knee will often again manifest its instability; resulting in repeat subluxation: this time often accompanied by cartilage damage and a visit to a doctor. The ACL tear is likelier to be accurately diagnosed at this second period of symptoms. Yet a third group of patients will feel better but still recognize that the knee is abnormal. These patients will not resume athletic activities but limit themselves to activities such as cycling or swimming or the use of an elliptical trainer which will be well tolerated. This group may do well for many years by adjusting their activities downward to avoid instability and relying more on their “good leg.” Many of these patients will nonetheless undergo gradual cartilage deterioration and present to a physician ten to twenty years after the intial injury with knee pain. Examination at this time will disclose the instability of ACL deficiency and often significant knee degenerative disease.
Physical Exam
Lachman Test : The Lachman Test is the best physical exam test for a torn ACL. The patient lies down on their back. The physician bends the knee to twenty degrees of flexion and stabilizes the thigh with one hand. He or she then pulls the lower leg forward with the other hand to see how much sliding or “anterior translation” occurs. This is compared to the normal knee. Substantially increased “translation” is diagnostic of an ACL tear. Unfortunately this test is very difficult to do and in the acute setting where muscle spasm and pain are present will often be falsely negative (i.e. normal) even though a tear is present. In the chronic setting where the knee is not inflamed and secondary stretching out of other supports has occurred the test is more reliable but still with a significant error rate.
Pivot Shift Test : The Pivot Shift Test involves attempting to get the knee to subluxate out of joint and then pop back. Unfortunately this is very painful, most patients can or will not cooperate with it and its main use therefore is in the anesthetized patient at the time of surgery to check the knee’s instability.
Hemarthrosis : Hemarthrosis means blood in the knee, usually associated with marked swelling. In an adult a hemarthrosis usually means an ACL tear is present although other conditions, such as fracture, can also produce this finding. In a child a dislocated kneecap will often produce hemarthrosis.
X-Rays: In most cases these are normal. In rare cases the patient will chip a piece of bone off the side of the tibia or where the ACL attaches which indicates ACL tear has occurred. These instances are however quite rare.
MRI : MRI is a good but not infallible test. In our published series we found a 19% false negative rate. I.E. 19% of the time the ACL was torn but missed by the MRI. Closed high field MRIs (usually 1.5 Tesla) are significantly more accurate than open low field units (typically 0.3 Tesla). If we obtain MRIs we therefore try to make sure they are closed high field MRIs. They are also highly dependent on an expert radiologist to interpret the results in addition to the orthopaedist. We have seen the same film interpreted as an intact ACL (wrong diagnosis) and a torn ACL (right diagnosis) by different radiologists on more than one occasion.
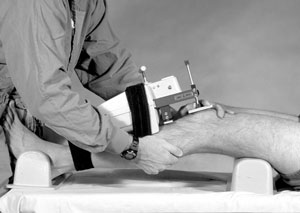 KT-1000 Arthrometer: This device is the most accurate means of diagnosing ACL tears. In the same published study from our center that found a 19% false negative MRI error rate, the KT-1000 was 100% accurate. To use it the surgeon performs a Lachman test on both knees but with this device attached. The test is painless, takes about ten minutes and is done by the surgeon in his exam room. It quantitates the difference in anterior translation between the two knees. The test is technically called an “instrumented Lachman” test. The normal knee typically has anterior translation of 3-7mm in response to what is called a maximum manual pull by the examiner. In the completely torn ACL the difference between the two knees will be more than 3mm and the reading on the affected side will usually be at least 10mm. Side to side differences of 1.5-3.0 mm typically occur with partial ACL tears. This is an expensive device that the surgeon must purchase. He or she must also be experienced in its use. There are also similar devices in use, particularly in Europe. We rely heavily on this device and do not routinely obtain MRI scans for ACL tears, since they are less accurate. We have found the KT-1000 useful in both the acute and chronic setting. If a patient has extensive muscle spasm the test will not yield accurate results, but it is generally easy to detect when such spasm is negating the results.
KT-1000 Arthrometer: This device is the most accurate means of diagnosing ACL tears. In the same published study from our center that found a 19% false negative MRI error rate, the KT-1000 was 100% accurate. To use it the surgeon performs a Lachman test on both knees but with this device attached. The test is painless, takes about ten minutes and is done by the surgeon in his exam room. It quantitates the difference in anterior translation between the two knees. The test is technically called an “instrumented Lachman” test. The normal knee typically has anterior translation of 3-7mm in response to what is called a maximum manual pull by the examiner. In the completely torn ACL the difference between the two knees will be more than 3mm and the reading on the affected side will usually be at least 10mm. Side to side differences of 1.5-3.0 mm typically occur with partial ACL tears. This is an expensive device that the surgeon must purchase. He or she must also be experienced in its use. There are also similar devices in use, particularly in Europe. We rely heavily on this device and do not routinely obtain MRI scans for ACL tears, since they are less accurate. We have found the KT-1000 useful in both the acute and chronic setting. If a patient has extensive muscle spasm the test will not yield accurate results, but it is generally easy to detect when such spasm is negating the results.
Conclusion: While the KT-1000 test is the most accurate means of detecting ACL tear: the history, exam, and MRI are also useful. The highest accuracy in diagnosis involves synthesizing the results of all of these means of detecting ACL tear.
Non Operative Treatment of ACL Tears
The overwhelming majority of ACL tears are treated surgically. If, however, a patient elects to not undergo surgical reconstruction there are certain principles that should be followed in planning their treatment. The most important consideration is the permanent avoidance of pivoting activities. Pivoting and landing after jumping are the two highest risk activities for inducing subluxations (“going out of place”) of the joint. This subluxation leads to accelerated degeneration of the joint due to cartilage damage. For exercise patients may walk, jog straight ahead, ride a stationery bike and swim. They should not play basketball, football, volleyball etc. because all sports put the knee at high risk of subluxation sooner or later. It is probably true that consciousness of the knee instability can allow the patient to keep the knee tense enough to prevent many of these episodes. However eventually if the patient is participating in these activities it is likely that they will forget to keep their knee tense and in the heat of the moment they will endure a subluxation episode. Thus avoidance of at risk activities is paramount.

The next most important consideration is strengthening of the muscles around the knee: especially the hamstrings. The hamstrings have a course that is somewhat parallel to the path of the ACL. Thus when they are contracted they essentially prevent knee subluxation. Quadriceps strengthening is also useful in keeping the knee together. Endurance is at least as important as strength as the knee must be kept tight for long periods of time.
Bracing may also be employed even though it has never been shown to be useful. It may be that a brace may be of some help if only as a reminder to the patient that their knee is defective.
It should be pointed out that knees with torn ACLs function abnormally even if they never experience “subluxation” episodes. It used to be thought that if these could be avoided then the knee might do well in perpetuity. However we now know that knees can continue to deteriorate and develop arthritis even if the knee never subluxates. This is an insidious process because the patient may have had a 5, 10 even a 20 year interval seemingly without a problem before pain develops – without subluxation. These knees often have significant articular cartilage damage even though the patient thought their knee was not at risk.
Arthritis Formation After Unreconstructed ACL Tears
The most important reason to reconstruct the ACL after it tears is to prevent the formation of degenerative arthritis of the knee. Because severe degeneration of the knee usually takes more than ten years to occur, many patients with unreconstructed ACLs are lulled into a false sense of security that their knee is not degenerating as described above. This can also occur with patients who have ACL reconstructions that have failed. If they do not have acute subluxations (“going out of place”) of the knee, they will be unaware that their ACL has failed until their degeneration produces pain. Evaluation at that time will disclose that the knee is unstable. Painful degenerated knees with torn ACLs or failed ACL reconstructions can be treated with various cartilage restorative procedures with a high degree of success. However it is far less traumatic to the patient and the outcomes are obviously better if the problem can be prevented in the first place.
Why and how do patients develop arthritis after ACL tear?
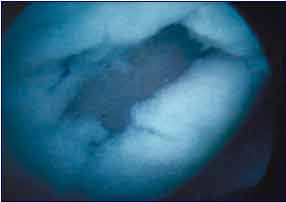 The Articular Cartilage: The knee without a functional ACL develops arthritis because the articular cartilage is damaged. Articular cartilage is the 3mm (variably) thick super-slippery and super-tough substance that coats the bones within all joints: allowing them to glide during movement without pain. Thinning and holes in this cartilage produce pain and inflammation and define what arthritis is. When this articular cartilage damage occurs the knee often develops stiffness in addition to pain. Articular cartilage, like central nervous system tissue and unlike for example skin or muscle tissue, cannot heal on its own. Articular cartilage damage after ACL tear occurs from three different mechanisms.
The Articular Cartilage: The knee without a functional ACL develops arthritis because the articular cartilage is damaged. Articular cartilage is the 3mm (variably) thick super-slippery and super-tough substance that coats the bones within all joints: allowing them to glide during movement without pain. Thinning and holes in this cartilage produce pain and inflammation and define what arthritis is. When this articular cartilage damage occurs the knee often develops stiffness in addition to pain. Articular cartilage, like central nervous system tissue and unlike for example skin or muscle tissue, cannot heal on its own. Articular cartilage damage after ACL tear occurs from three different mechanisms.
- First, the ACL deficient knee has abnormal mechanics during all movements. This results in a gradual wearing down of the articular cartilage of which the patient is usually unaware.
- Secondly, in many, but not all cases there are “subluxation” (partial dislocation) episodes when the knee “goes out of place.” These very painful episodes can result in accelerated articular cartilage attrition, or can result in large chunks of the articular cartilage being scooped away from the bone (similar to what occurs when a golfer takes a “divot” of grass from the ground when hitting a golf ball.)
- The third mechanism is as a result of “meniscal” tears. In addition to direct damage to the articular cartilage, the articular cartilage is indirectly damaged when meniscal tears occur. Each knee has a medial meniscus and a lateral meniscus (hence two menisci). These structures are torn at much greater rate in ACL deficient knees. They are wedge shaped shock absorbers that are made of a combination of cartilage and “fibrous” tissue (found for example in scars). They provide cushioning that protects the articular cartilage. When the menisci are torn, this cushioning function is diminished and the unprotected articular cartilage wears more quickly. The menisci will often continue to tear until very little is left unless the knee is stabilized by ACL reconstruction.As the articular cartilage is damaged it wears down further and further until pain is eventually felt. This pain usually does not occur until the cartilage is severely worn through so that the patient will typically damage the knee for ten years or more before they realize this is happening. Often the patient will be quite active during this time not realizing that their increased activity level is hastening the degeneration of their knee.
- Malalignment: Arthritis is further accelerated in knees with what is called either “varus” (“bow-legged”) or “valgus” (“knock-kneed”) alignment. In varus knees the medial (inner) compartment has increased stresses on it and any abnormality in the joint, such as a torn ACL and even more-so a torn medial meniscus, will result in greatly accelerated degeneration of that compartment. The same process can occur in the lateral compartment in a valgus knee and again especially with a torn lateral meniscus. The menisci are so important in joint preservation that in some cases it is necessary to transplant a cadaveric meniscus into the knee when pain first appears to try to prevent severe arthritis from developing. Varus and valgus is often not noticeable when looking at the knee and can only be accurately measured using special long x-rays called mechanical axis views. In the normal knee a line drawn from the center of the hip to the center of the ankle will pass through the center of the knee. In a varus knee this line passes through the medial (inner) side of the knee causing greatly increased stresses there during walking. In a valgus knee the stresses are concentrated on the outer side of the knee. The amount of this malalignment can be quantitated by measuring the angle formed between two lines: the first is a line connecting the center of the hip and knee, the second is a line connecting the knee and ankle. This mechanical axis should be zero. The more it deviates from zero the greater will be the effect of the loss of cushioning from a torn meniscus. When the angle is more than four degrees of varus in a degenerating knee it is necessary to perform a procedure called “high tibial osteotomy” to correct the alignment. Varus is roughly ten times more common than valgus. It should also be noted that many athletes with good footspeed have varus knees (notice the number of such knees in running athletes such as wide receivers in football). Thus many athletic people are particularly prone to especially rapid degeneration of their knee after ACL tear and medial meniscal tear because of this varus malalignment.
Does ACL Reconstruction Really Prevent This Arthrosis? This is a controversial topic. Earlier studies seemed to show that it did not help much. However these earlier ACL reconstructions often did not effectively stabilize the knee. More recent studies with more effective ACLR show that ACLR is effective in slowing down and possibly preventing this degeneration from progressing.
The Economics of ACL Reconstruction
- ACL reconstruction is paid for by all major insurance companies. The procedure is now typically performed on an outpatient basis.
 Ice Machines that electronically circulate ice-water through a pad applied to the knee at surgery are very effective in relieving pain. Formerly they were routinely reimbursed but most insurance companies no longer cover them. The patient thus either must use ice bags applied to the knee or pay two to three hundred dollars out of pocket.
Ice Machines that electronically circulate ice-water through a pad applied to the knee at surgery are very effective in relieving pain. Formerly they were routinely reimbursed but most insurance companies no longer cover them. The patient thus either must use ice bags applied to the knee or pay two to three hundred dollars out of pocket. Braces are used in the early post-operative phase by most surgeons and are typically covered.
Braces are used in the early post-operative phase by most surgeons and are typically covered.- Continuous Passive Motion Machines are used by some surgeons to attempt to increase motion and possibly reduce pain. Because the scientific literature has not shown them to be effective many insurers no longer cover them for ACLR. We have not found them necessary for ACLR itself but do use them when performing cartilage regenerative procedures such as ACI or microfracture.
- Physical Therapy is necessary after ACLR and is reimbursed by insurance. However the extent of coverage varies widely and must be closely checked before beginning to make sure that benefits do not run out before treatment is completed. The amount and type of therapy also varies widely depending on the type of procedure performed, the surgeon’s experience and preferences, and how the patient progresses after surgery.
Graft Choice and Graft Strengths For ACLR
The injured ACL does not heal if the surgeon attempts to sew it back together: i.e. to repair it. This approach was tried for decades until it was realized in the 1980′s that the only consistently successful approach is to fashion a new ligament using a graft.
Graft Types: Grafts may be categorized as “autografts,” “allografts, ” and “synthetics”. Synthetics, such as Dacron or carbon fiber were tried in the 1980′s and 1990′s but had poor results and have been almost completely abandoned. The gold standard for ACLR is an autograft of one kind or another. Allografts are also used. Some surgeons have had good success with their use but overall success rates have been lower. We will discuss each of the common autografts and allografts in common use below.
Pros and Cons: Autografts
Hamstring Autograft: The semitendinosus with or without the gracilis tendon is commonly and increasingly used for ACLR. This is the graft I use. The benefits of this graft are that it is the strongest autograft available, roughly 50% stronger than a patellar tendon autograft for example. In addition patients routinely have full restoration of hamstring strength by the time they are ready to return to sports. The primary hamstrings are the semimembranosus and biceps femoris muscles and they are left intact and grow a little stronger to compensate for the semitendinosus which is an accessory hamstring. It is now also clear that the semitendinosus tendon actually regrows back to its original location in more than 90% of patients. The gracilis tendon is not a hamstring but an adductor. It too is only an accessory muscle with the main adductors being the adductor magnus, longus and brevis providing most of the adductor torque and taking over its function when the gracilis is used. We published a “meta-analysis” in 2005 in the journal Arthroscopy in which we reviewed all scientific papers that compared hamstring grafts with patellar tendon grafts and found that while both gave good results, the overall stability was higher with the hamstring grafts and the overall failure rate was lower.
 Patellar Tendon Graft: This graft is used by many surgeons and in the hands of surgeons skilled in its use has produced very good results. While it is not as strong as a hamstring graft it is strong enough to restore good stability in most cases. Its use has been declining markedly in recent years because there is an increased incidence of kneeling pain and frontal knee pain after its use. Many surgeons who like this graft have now turned to patellar tendon allograft to avoid the problem of kneeling pain in recent years. However some of the best ACL surgeons continue to use it with excellent results.
Patellar Tendon Graft: This graft is used by many surgeons and in the hands of surgeons skilled in its use has produced very good results. While it is not as strong as a hamstring graft it is strong enough to restore good stability in most cases. Its use has been declining markedly in recent years because there is an increased incidence of kneeling pain and frontal knee pain after its use. Many surgeons who like this graft have now turned to patellar tendon allograft to avoid the problem of kneeling pain in recent years. However some of the best ACL surgeons continue to use it with excellent results.
Quadriceps Tendon Graft: This is a more recently described graft. It has produced good results without the high incidence of kneeling pain seen with patellar tendon grafts. Because only a few surgeons routinely use it there is less scientific literature concerning it. Perhaps for this reason it is not yet widely used. However in the hands of surgeons skilled in its use it has produced very good results. Its strength appears to be a little greater than bone-patellar-tendon-bone (patellar tendon) graft but significantly less than four strand hamstring graft.
Pros and Cons: Allografts
Tibialis Allograft : This graft is similar to hamstring autograft in the way that it is fixated in the knee. It has become increasingly popular although there is very little scientific literature describing its efficacy because it is so new.
Patellar Tendon Allograft : As mentioned above, the proponents of this graft believe they achieve high efficacy without the kneeling pain seen with the autograft. There are several repots in the scientific literature showing its use. There have been excellent results reported and some reports with lower efficacy. In a meta-analysis we performed comparing autografts and allografts there was a lower overall rate of stability with patellar tendon allograft when compared to autograft.
Achilles Tendon Allograft: This graft is used by some but again there is very little literature showing success rates. A recent report showed lower success rates than with other grafts which seemed to correlate with increasing age of the donor from whom the graft was taken.
SummaryEfficacy: In our meta-analysis we found an overall lower rate of stability with allograft use when compared with autograft although some surgeons have had very high success rates with allografts
Infection: One study showed a higher infection rate with allografts when compared with autografts although many surgeons have reported series with no infections. We have not had a deep knee infection since we began using our current technique in 1992. While it is only anecdotal information I have recently seen two cases of infected allografts referred to our clinic.
Disease Transmission: The incidence of disease transmission is very low but hepatitis and bacterial infections have been transmitted recently. One death occurred from such a disease transmission in 2002. Unfortunately techniques that can sterilize allografts, such as high dose radiation, have also been shown to weaken them. Thus most allografts are implanted today without being sterilized. They are harvested under sterile conditions which is adequate in most cases. However unscrupulous individuals recently harvested many grafts from funeral homes without sterile technique and then passed them off as sterile grafts to tissue banks – as was widely reported in the media in 2006. This points out the added level of vulnerability involved in allograft use versus autograft.
ConclusionThe most important factor in graft choice is the experience and results of the surgeon using that graft. It is much more important that surgeons have good success and skill with the graft than which graft they use. Having said that there is consensus within the orthopaedic community that the gold standard for ACLR is autograft at this time.
Synthetic Ligaments
In the farther off future it is likely that “off the shelf” ligaments may be seeded with a patient’s own cells and implanted in the knee: thus obviating the need for autografts or allografts. Efforts have been undertaken in this regard for over 20 years. Indeed carbon fiber ligaments were implanted in thousands of patients, primarily in Europe, in the 1980′s in the hope that they would behave in this fashion. Unfortunately, such attempts to date have been generally unsuccessful.
Fixation Devices In ACLR
ACL grafts grow into bony tunnels within the knee. This process takes two to three months after surgery. During this time they must be held rigidly in place so that they do not loosen. To accomplish this there are a myriad of fixation devices in current use. Each surgeon chooses the device that he or she feels is the most efficacious and that he or she has the most skill using. This is a decision that should be left up to the surgeon. However there are some questions about fixation devices that we encounter that are of general interest to the patient.
 Metal Versus Bioabsorbable: Initially, virtually all fixation devices were made of metal: stainless steel or titanium. More recently bioabsorbable plastics have been used. A small benefit of their use is that they do not distort mri’s that might be done near to where they have been implanted as metal screws can. But the primary benefit of using these devices was supposed to be that they would dissolve and be replaced by bone. However it has recently become clear that these devices may not be beneficial after all. This is because it has been found that the devices often take more than five years, instead of one or two years to be reabsorbed. More importantly it appears that when the devices reabsorb, bone probably does not grow in to take their place as originally assumed. Rather it appears that there probably remains a kind of plastic sludge where the screw used to be. This would actually be a potentially worse situation than having a metal screw in place because the sludge would represent a potential weak spot in the bone whereas the metal in bone – like reinforced concrete – would not produce a weakened area. This is all theoretical since there have been no reported adverse events associated with these bioabsorbable screws. And there are even newer devices that are specifically designed to produce bone when they do reabsorb. However they are quite new, and as with the plastic devices, it will be years before the reality is known. The conclusion however is that both metal and plastic devices have produced good results and there have been no adverse events reported that are specifically referable to the composition of the device. The most important factor is the surgeon’s comfort level with whatever device he or she chooses.
Metal Versus Bioabsorbable: Initially, virtually all fixation devices were made of metal: stainless steel or titanium. More recently bioabsorbable plastics have been used. A small benefit of their use is that they do not distort mri’s that might be done near to where they have been implanted as metal screws can. But the primary benefit of using these devices was supposed to be that they would dissolve and be replaced by bone. However it has recently become clear that these devices may not be beneficial after all. This is because it has been found that the devices often take more than five years, instead of one or two years to be reabsorbed. More importantly it appears that when the devices reabsorb, bone probably does not grow in to take their place as originally assumed. Rather it appears that there probably remains a kind of plastic sludge where the screw used to be. This would actually be a potentially worse situation than having a metal screw in place because the sludge would represent a potential weak spot in the bone whereas the metal in bone – like reinforced concrete – would not produce a weakened area. This is all theoretical since there have been no reported adverse events associated with these bioabsorbable screws. And there are even newer devices that are specifically designed to produce bone when they do reabsorb. However they are quite new, and as with the plastic devices, it will be years before the reality is known. The conclusion however is that both metal and plastic devices have produced good results and there have been no adverse events reported that are specifically referable to the composition of the device. The most important factor is the surgeon’s comfort level with whatever device he or she chooses.
Interference Screw Versus Cortical Fixation: Interference screws are inserted within the bony tunnels and hold the graft by friction. Cortical devices sit on the outer surface of the bone and anchor the graft from that location. In our 2005 meta-analysis on this subject we found that both are efficacious. We found slightly higher overall stability rates with cortical devices than interference devices (and some surgeons will back up interference devices with cortical devices which was found to be highly effective) but excellent results, and less than excellent results, were obtained with all categories of devices. Again it is the surgeon’s skill, comfort and experience with a given device that is most important. There are complicated theoretical advantages and disadvantages to each device, and the final answers are not yet in.
One of the main findings of our study was that cortical devices were possibly even more effective, but certainly as effective, as interference screws. We have used cortical devices exclusively with our hamstring grafts with high success rates. In general interference screws are used more often with patellar tendon grafts and cortical fixation more often with hamstring or other soft tissue grafts. But again excellent results have been obtained with every conceivable combination of graft and fixation device.
Do Fixation Devices Cause Pain and Should They Be Removed?: Fixation devices do not need to be removed unless they cause pain. Overall the incidence of fixation devices causing pain is very low and they are seldom removed
How Often Do Fixation Devices Fail?: The overall incidence of fixation device failure or breakage is exceedingly low. These events do occur rarely and may require another procedure to rectify.
Ligamentization and Graft Tunnel Healing
Ligamentization: Whether autograft or allograft, all ACL grafts are tendons. Tendons are similar to, but different from, ligaments. Both are composed of fibrocytes in a collagenous matrix. However the microanatomy differs. In particular the sizes of the fibers within tendons and ligaments differ. When tendons are use to replace the ACL they undergo a process that has been called “ligamentization” in which the microanatomy becomes more ligament-like and less tendon-like. This process takes years to complete. When grafts are first put in they undergo a period of substantial weakening in which they can lose up to 80% of their initial strength. This corresponds to a period of swelling when they are developing a new blood supply. It is partially because the grafts are weak during this time that it is important to protect new grafts during the first few months after surgery. There is controversy concerning this subject within the orthopaedic community and some feel that this weakening does not occur. These surgeons tend to provide more aggressive rehabilitation during this period. There is more and more evidence however supporting caution during this period. We have long advocated protecting the graft during this period while still performing exercises to avoid stiffness and muscle atrophy. This can be safely done but requires a high level of skill and awareness on the part of the physical therapist to gain the benefits of therapy without compromising the graft
Graft Tunnel Healing: The graft takes from six to twelve weeks to fully implant within the bony tunnel. On average soft tissue grafts such as hamstring grafts take a few weeks longer than bony grafts such as patellar tendon: but the ultimate strength of the attachment of the graft to the bone is ultimately the same with both types of grafts. During this time the graft should be protected so that it does not slide in the tunnel and become loose. Again, surgeons vary on the degree of aggressiveness which they think the graft will tolerate during this time and the intensity of the therapy they prescribe.
Allografts: Allografts clearly “ligamentize” more slowly than autografts. Thus it is important that they be carefully protected in the postoperative period to prevent loosening. New cells and blood vessels grow into all ACL grafts and this process takes longer to accomplish in allografts. There is some evidence that even years after surgery it may not be complete. There is also some evidence that graft-tunnel healing may take place more slowly. It has been suggested but not proven that allografts have a higher rate of late failure – years after surgery – than autografts for this reason.
Revision ACLR:Reconstruction After Failed Initial Surgery
ACL Failure Rate: In our meta-analysis published in 2005 we found that the overall rate of failure of the graft after ACLR in the hands of the worldwide authorities who were the authors of the papers analyzed – was about 5%. It is estimated that the overall rate in the community in the United States is in the ten per cent range or higher. (The failure rate at our center was zero per cent from the period 1992 when we began keeping statistics.) Assuming about 125,000 ACL reconstructions will be performed this year in the U.S. this would mean that there would be an annual rate of perhaps 12,000 revision procedures required.
Differences In Revision Patients: On average these patients will have a higher rate of cartilage damage than patients undergoing an initial ACL reconstruction because they have had prolonged instability due to their graft failure. Because they have implanted hardware devices and tunnels that may have enlarged or be in the wrong place, revision surgery is far more difficult than primary surgery.
Results After Revision Surgery: In the hands of experienced surgeons excellent stability results can be obtained in revision ACL surgery. Despite this, the average revision patient will have a lower level of function than the average primary patient. This is because of the higher rate of cartilage damage and degenerative disease in these patients.
Technical Challenges In Revision Surgery:
- Bone Tunnels: The bone tunnels may not be in the right location for the revision surgery or may have widened as frequently occurs after even successful surgery. If the tunnels are thus rendered impossible to use, the revision surgeon will need to bone graft these tunnels and allow them to heal for four to six months before proceeding with the implantation of a new graft. This bone graft is most commonly taken from pelvic bone on the same side and can usually be accomplished arthroscopically in the knee and through a mini-incision in the hip area that is well hidden by clothing. This is an outpatient procedure with immediate partial weight bearing. When the bone graft is mature the surgeon returns and carries out a conventional ACLR.
 Old Hardware: Unless bioabsorbable implants were used, the patient may have remaining metal hardware: interference screws, cross pins or other devices. In general it is best to leave these devices in place unless they are in the way of the new procedure. This is because removing them leaves a weak area in the bone that takes years to fill in. Also it may weaken the bone adjacent to the hardware thus potentially causing a new tunnel to collapse. Finally when removing these implants often healthy bone must be removed with them in the process of excavating them. However if the old implants are in the way then the surgeon will remove them and decide whether or not this necessitates a bone graft at that time.
Old Hardware: Unless bioabsorbable implants were used, the patient may have remaining metal hardware: interference screws, cross pins or other devices. In general it is best to leave these devices in place unless they are in the way of the new procedure. This is because removing them leaves a weak area in the bone that takes years to fill in. Also it may weaken the bone adjacent to the hardware thus potentially causing a new tunnel to collapse. Finally when removing these implants often healthy bone must be removed with them in the process of excavating them. However if the old implants are in the way then the surgeon will remove them and decide whether or not this necessitates a bone graft at that time.- Graft Choice: Either autograft or allograft may be used. This depends on what was used the first time and what the surgeon’s preferred graft is. We use hamstring autograft for our cases. If this is the graft that failed and is thus unavailable because it has already been harvested we use the hamstring from the opposite leg. This can be operated through tiny incisions that produce little pain. Patients are able to walk on that leg and go home the day of surgery. As with all ACL surgery the choice of graft should be the graft that the individual surgeon feels produces the best results in his or her hands. Excellent results can be obtained with any graft if the surgery is well done.
- Associate Cartilage Restorative Procedures: Since more revision patients will have degenerative changes there is a greater need for cartilage restorative procedures in this population such as microfracture, autologous chondrocyte implantation, meniscal allograft transplantation, high tibial osteotomy and osteochondral allograft implantation. This adjunctive surgery can be sometimes done simultaneously with the revision ACL surgery or may be done on a staged basis. These are complicated cases and must be individualized. Simultaneous surgery is easier on the patient because there will ultimately be fewer surgeries, but more complicated surgeries also carry a higher risk of stiffness. Obviously it is best to err on the side of safety over expediency.
ACLR In Children Who Are Still Growing
Incidence and Definitions: The overwhelming majority of ACL tears occur in persons who have stopped growing. This usually occurs at 15.5 years of age in boys and 14.5 years of age in girls. This is however subject to wide variation. It is checked by taking an x-ray of the affected knee and also an x-ray, if there is any question, of the affected left hand (“bone age” is standardized to left hand x-rays in an atlas). People who are still growing are called “skeletally immature.” Their growth plates are “open.” When growth is done the growth plates are “closed.”
Risks of Surgery In Growing Children: Improper surgery when the growth plates are open can result in premature cessation of growth in the knee and also asymmetric growth producing bending of the bone as it grows. However, as we will discuss, appropriate surgery can be safely performed when the growth plates are open.
Alternatives:
- Waiting: One alternative would be to not operate until the growth plates are closed. This is however a dangerous proposition because studies have shown that children in whom surgery is forestalled have an even higher incidence of cartilage damage and degenerative arthritis formation during the waiting period than adults. This is because children’s joints are looser and because children are more active and less cautious than adults. In addition waiting necessitates complete abstinence from any pivoting activities. This can be quite psychologically stressful on a child. It is also unlikely the children will cooperate with such a regimen.
- Surgical Reconstruction: Surgery can be carried out with minimal risk if certain principles are followed. If the growth plate is drilled across carefully and if no fixation crosses the growth plate and if a soft tissue and not a bony graft is used studies have shown virtually complete safety. There is also a specific technique that does not cross the growth plate at all providing an even greater measure of security. In either case the surgery is more difficult than conventional ACL surgery and must be carried out by an experienced ACL surgeon. We believe that it is safer for the child to have appropriate reconstructive surgery within the first few months after injury than to risk cartilage damage and degeneration by postponing surgery for a prolonged period.
The Treatment of Partial ACL Tears
Incidence: Partial tears are much less common than complete tears. The true incidence is unknown but probably only about 10% of all ACL tears are partial tears.
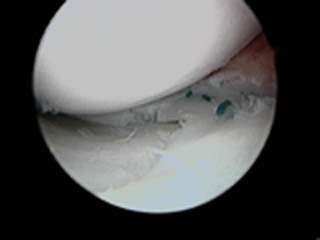
Diagnosis: The mechanism of injury and diagnosis are similar to complete ACL tear. In the awake patient the KT-1000 is the best means of diagnosis. If the diagnosis is not clear the patient can undergo an examination under anesthesia in which the pivot shift test determines whether the knee is going out of place, subluxating, or not. The MRI has poor differentiating power for both partial tear versus normal and for partial tear versus complete tear. Arthroscopic examination may be less accurate than the pivot shift test and the KT 1000 arthrometer. The reason is that a partially torn ligament visually (i.e. as seen through the arthroscope) may or may not have significant stabilizing power for the knee. This can be better evaluated using functional tests such as the pivot shift and KT-1000. That is, arthroscopic examination is good for telling if the ACL is completely torn or completely normal but for partial tears has less ability to determine whether the part of the ligament that is not torn is capable of stabilizing the knee.
Treatment: In a true partial tear the results are usually good with non-operative treatment. Since the ACL is stretched as the knee is fully straightened, it is worthwhile to keep the patient on crutches for 3-4 weeks with the knee mobile but blocked from fully extending, to allow the ACL to heal without tension – which will presumably give it the best chance to heal taut. After this, activities should be protected for another 2-3 months to allow maximum healing to occur. In our experience most patients will do well with this regimen including successful return to competitive sports. Such patients are at increased risk of complete rupture in the future and if this occurs at a later time formal reconstruction can be undertaken then.
Partial Tear Repair: Recently some surgeons have attempted to reconstruct the part of the ACL that tore without disrupting the part that remains. This is being done by only a few surgeons and it remains to be seen if it will be beneficial. There are concerns that it will be difficult to reconstruct the torn part without damaging the previously undamaged part.
Complete Reconstruction: We believe this is not indicated for partial tears with les than 3mm side to side KT 1000 asymmetry unless the patient is having instability or subluxation episodes. It would involve destroying a functioning, if somewhat compromised, ligament to make room for a new graft.
Rehabilitation: Strengthening of the knee, particularly the hamstrings is beneficial.
Bracing: This is the only circumstance in which we recommend a brace be worn during sports. There is no evidence that a brace is beneficial in any setting, but we believe that the risk-benefit ratio does favor its use with partial tears.
Do Partial Tears Lead To Arthritis? The answer to this question is not known but we believe that in general partial tears are well tolerated with much less of a tendency to produce arthritis than complete tears.
Treatment of Associated Injuries
 Both cartilage and other ligament injuries can be associated with partial ACL tears. These will be addressed individually.
Both cartilage and other ligament injuries can be associated with partial ACL tears. These will be addressed individually.
Torn Meniscus: The torn pieces should be trimmed when they are seen unless they are in the small peripheral zone which is amenable to repair. Meniscal repair should then be carried out. The incidence of stiffness is higher after ACLR when a meniscus is concomitantly repaired in a locked knee. For this reason when this occurs some surgeons prefer to first repair the meniscus, regain full motion and then go back one or two months later to repair the ACLR.
Full Thickness Articular Cartilage Defect: If these lesions are under 2 square centimeters in size we treat them with microfracture at the time of the ACLR. If they are larger we take the articular cartilage removed normally during ACLR from the intercondylar notch (notchplasty) and send it to Genzyme biosurgery in Cambridge Massachusetts. There the cells are isolated, grown to a much larger volume and frozen. They are then flown back a few months later for implantation into the site of the articular cartilage defect. This procedure is called “autologous chondrocyte implantation“.
Medial Collateral Ligament Tear (MCL): In most cases this injury can be ignored. In some cases it will heal spontaneously. In others some persistent side to side laxity will remain. However studies have shown that repair does not improve results and indeed overall results tend to be worse because stiffness and pain can occur when repair is attempted.
Lateral Collateral Ligament Tear (LCL): These must always be repaired or reconstructed when they occur, generally as a separate procedure. However this injury is exceedingly rare.
Posterior Cruciate Ligament Tear (PCL): This ligament can also heal on its own. We therefore reconstruct the ACL and then observe to see if the patient is having symptoms. In general patients do not have symptoms and do not need reconstruction of the PCL once the ACL is reconstructed assuming the medial and lateral collateral ligaments are also intact. If the patient does have symptoms the PCL can be reconstructed. It should be pointed out however that the results of PCL repair are not consistently good. In addition, best results for PCL reconstruction are felt by some to require open surgery, rather than minimally invasive arthroscopic surgery as is done for the ACL. Because there are few if any problems in not fixing the PCL and because the surgical alternatives do not produce consistent results and are extensive to perform, we usually find it unnecessary to reconstruct the PCL.
Malalignment and Arthritis: If the patient has early arthritic changes in the medial compartment of the knee and also has a varus (bowlegged alignment) knee we will recommend simultaneous or sequential high tibial osteotomy. This procedure is highly effective in relieving early arthritic pain and allowing some regeneration of articular cartilage. If the patient has lateral compartment arthritis he can have distal femoral osteotomy to correct this problem.
Post Operative Course and Rehabilitation
Goals: The goals of rehab are the restoration of motion and strength without compromising stability.
Motion: We allow early motion in a brace and begin therapy three or four days after surgery. Nuances of various regimens vary but most surgeons avoid prolonged immobilization which can promote stiffness.
Hyperextension: Hyperextension is the straightening of the knee past full straightness so that the knee bends “backward” a small amount, usually about five degrees. Some surgeons advocate hyperextension and feel it avoids stiffness and frontal knee pain. However we have not found it necessary to use hyperextension to achieve these goals. And since hyperextension strains the graft we specifically avoid it until full return to function at six months to avoid graft loosening.
Weight Bearing: Most surgeons begin weight bearing soon after surgery: some on the same day. We begin weight bearing on the third or fourth post-operative day for reasons of comfort. Crutches are important to allow the patient to walk without pain and without a limp. The normal gait pattern provides the new ACL with mechanical and electromagnetic signals that facilitate post-operative ligament healing at the cellular level. We progress from two crutches to one to none over the first three to four weeks on average after surgery. Patients progress at their own individual pace. Our mantra during this time is “no pain, no limp.” That is, the patient should take as much weight off their knee as necessary during this time so that they do not limp and do not experience knee pain.
Knee Bracing: We, like most surgeons, apply a brace at the end of the surgical procedure. We have found that patients in general feel more secure with the brace in place. However we discontinue the brace as soon after surgery as the patient feels comfortable. No further bracing is needed when the patient returns to full activities. Some surgeons do recommend later bracing. 
Strengthening: Surgeons vary most in this parameter. We begin an early quadriceps exercise called the 90/90 wall push that is effective in avoiding quadriceps atrophy without strengthening the ligament. It is important to note that exercises that use an active quadriceps contraction put a tremendous strain on the ACL unless the knee is kept in greater than fifty degrees of knee flexion during the exercise. We avoid repetitive motion activities such as cycling until the end of the third post-operative month when the graft has its new blood supply well established to avoid graft abrasion. We also begin early hamstring strengthening.
Proprioception: Proprioception is another name for “position sense” This is the sense that allows you to, for example, close your eyes and touch your finger to your nose without looking at it. Your body has an innate sense of where its various components are in space without the use of vision. It is believed that proprioception is at least partially mediated through sensory nerves in the ACL. To facilitate return of function in this regard we perform specific proprioceptive, position sense, exercises after surgery: although it is unclear at this time how effective these exercises are.
Graft Protection: As described in the chapter on “ligamentization and graft tunnel healing” the graft and its attachment sites are quite fragile in the early post operative period. We therefore make protection of the graft during this three month period after surgery our highest priority. We emphasize return of motion and function but not exercise so as not to cause damage or loosening of the graft. During the second three month period we emphasize return of strength and cardiovascular fitness. By the end of this period, six months post-operatively, well over 90% of our patients have full restoration of strength and function and can resume all activities at an unrestricted level. Some surgeons believe it is advisable to be more aggressive earlier to avoid stiffness. However we have not had problems avoiding stiffness and protecting the graft at the same time as described.
Restoration of Hamstring Strength
As mentioned above in chapter 9 full restoration of hamstring strength is achieved by six months in almost all cases. The main hamstring muscles, the semimembranosus and biceps femoris become stronger to take over the function of the semitendinosus. And studies have shown that in over 90% of cases the semitendinosus eventually grows back after it is resected for use as an ACL graft.

Results: This regimen has allowed us to achieve a 100% level of graft patency (that is a zero per cent graft failure rate) since we began using this technique in 1992, and still allow full restoration of early motion and then strength by six months post-operatively on a routine basis.
Video: A video describing this rehabilitative regimen may be viewed on our ACLR Rehabilitation page. Some surgeons, particularly those using the patellar tendon autograft, advocate a more aggressive approach.
Stability Results After ACL Reconstruction
 Introduction: We performed and published the most extensive work to date comparing the stability results after ACL reconstruction. This meta-analysis pooled data from patients with hamstring and patellar tendon grafts and compared them. We then extended the study to include allografts. We will present the main points of this data here but it is important to realize that these are only averaged results. Individual surgeons have widely varying results using the same technique based on their skill at performing the procedure. The stability was based on analysis of KT 1000 data. The terms used are “normal stability” which means that the operated knee was within 2mm as stable as the normal opposite knee, and “abnormal stability” which generally corresponds with failure of the graft and corresponds to a side to side difference of greater than 5mm using the KT 1000.
Introduction: We performed and published the most extensive work to date comparing the stability results after ACL reconstruction. This meta-analysis pooled data from patients with hamstring and patellar tendon grafts and compared them. We then extended the study to include allografts. We will present the main points of this data here but it is important to realize that these are only averaged results. Individual surgeons have widely varying results using the same technique based on their skill at performing the procedure. The stability was based on analysis of KT 1000 data. The terms used are “normal stability” which means that the operated knee was within 2mm as stable as the normal opposite knee, and “abnormal stability” which generally corresponds with failure of the graft and corresponds to a side to side difference of greater than 5mm using the KT 1000.
RESULTS: The results are summarized in the following table.
GRAFT |
NORMAL STABILITY |
ABNORMAL STABILITY |
HAMSTRING |
76.6% |
4.4% |
BONE-PATELLAR TENDON-BONE |
66% |
5.9% |
ALLOGRAFTS |
59% |
14% |
OUR RESULTS |
86% |
0% |
These results show Hamstring to have a slightly higher stability rate than patellar tendon and allograft to have a substantially lower stability rate than both autografts. Our results with hamstring were slightly better than the overall stability rate with hamstrings but were the same as others using hamstring grafts and the type of fixation we use (this data is presented in our published paper on this subject). Again however we wish to emphasize that excellent results have been obtained by some surgeons using all of these different types of grafts and this published data averages the results from 84 published series that met the criteria for inclusion in the study. These results are obtained from surgeons who are experts in this procedure and probably represent best case results for this reason. Thus the overall five percent abnormal or failure rate with autografts is estimated to be ten per cent or more if all reconstructed knees are considered.
Complications and Problems
Infection: The infection rate after ACLR is quite low. For autografts it is less than 1% of cases. One study compared autografts to irradiated allografts to non-irradiated allografts. It found that the rate for non-irradiated allografts was 4% whereas the rate for autografts and irradiated allografts was under 1%.
Graft Failure: As mentioned above this rate is probably as high as 10% overall although it will vary significantly from surgeon to surgeon.
Stiffness: The incidence of knees with significant loss of motion is generally less than 5%.
Frontal Knee Discomfort: The incidence of this problem has been found to be as high as 45% with patellar tendon grafts and 20% with hamstring grafts and allografts. It manifests as discomfort with kneeling, squatting and stair climbing. It is usually not severe but can inhibit full return to activities. It is probably multi-factorial and efforts to further diminish it are ongoing.
Osteoporosis: Researchers in Sweden have found that some degree of bone softening occurs in both legs after ACL reconstruction. The reasons are unclear and specific treatment regimens have so far not been effective. Fortunately this finding has not been associated with adverse clinical events.
Deep Vein Thrombosis: There is a small but definite incidence of DVT or blood clot after ACLR. In the United States most surgeons have not prescribed blood thinners to address this problem, unless the patient is at known high risk, since it has not proven to be a significant clinical problem and blood thinners have their own set of complications to weigh against any good they may do.
Numbness: This is found in about two thirds of the patients who have knee surgery of any kind as a result of the incision and dissection under the skin. It is partial numbness, it diminishes with time and is seldom a significant clinical problem. We are finishing a research study based on cadaver dissections and a modified surgical technique that has been effective in reducing the incidence of numbness.
Fixation Device Problems: Problems with these devices are rare. There have been occasional reported episodes of breakage requiring re-operation. Also rarely the devices may cause pain requiring removal.
Fracture: There have been a few reported instances of fracture through the bone tunnels.
Tunnel Widening: It has been noted for some time that tunnels through which the grafts are passed tend to widen during the first year after surgery. Typically these tunnels are roughly 9mm in diameter and may widen one or two extra millimeters. The cause is uncertain and no adverse clinical event has ever been described as a result. This widening may increase the need for bone grafting if later revision surgery is necessary.
Tissue Engineering
Growth Factors : Tissue engineering refers primarily to the use of growth factors or biological enhancements to improve the results of medical treatment. In the case of ACL reconstruction there are biological factors that have shown promise in animal studies in increasing the speed of healing and the strength of ACL grafts. In the next five to ten years it is likely that clinical trials in humans will be started.









